1162 visitors from Jan 2013
International collaborative group aiming to create, support and disseminate research in cardiovascular field providing CRF web-based platforms for multicenter studies
Coordinator and creator: Enrico Cerrato; Fabrizio D'Ascenzo
Scientific Board: G.Biondi-Zoccai; J.Escaned; C.Moretti; G.Campo; I.Sheiban; C.Templin; I.Nuñez-Gil; S.Raposeiras Roubín; W.Wojciech; L.Perl; F.Varbella
Injeneering: D.Gallo; U.Morbiducci
Read News
Cardiovascular Disease in HIV patients: From Bench to Bedside and Backwards - Dr E.Cerrato
Since 1998, when Keith Henry, in a letter to The Lancet, reported two cases of myocardial infarction in young HIV men on protease inhibitors (PIs), a large bulk of evidence, derived both from randomized trials and from observational cohorts proved the increased risk of myocardial infarction in patients on highly active antiretroviral treatment (HAART). Despite the recognition of this risk, only in the last decade several studies have assessed the underlying histopathology and impact of this condition on worldwide cardiovascular health.
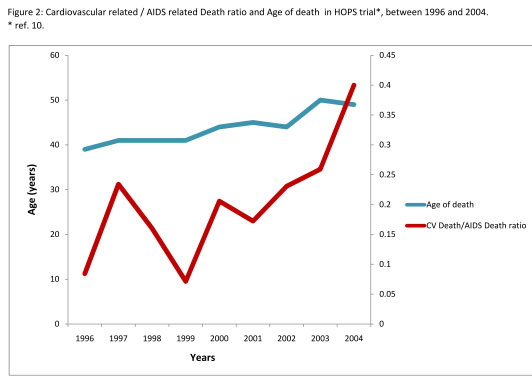
The HOPS and DAD trials, two large prospective observational cohort studies
conducted between 1996 and 2008, have shown that HIV-infected patients receiving
HAART have considerably longer life expectancy with early recognition and treatment
(similarly to HIV-negative subjects), thus increasing the life span for HIV-related
chronic comorbidities including cardiovascular, renal and bone diseases. A premature
ageing process and a high prevalence of comorbidities (and therefore treatment
with several medications) have been described and contribute to the increased
frailty and mortality that are recognized in HIV-positive subjects. Furthermore,
antiretroviral drugs (ARVs) have been associated directly with increased cardiovascular
risk (such as abacavir or PIs) or to imbalances in several cardiovascular risk
factors (such as insulin resistance and dyslipidemia). The increasing availability
of ARVs, the improvement in life expectancy and risk factors prevalence together
with the growing “westernization” of sub Saharan African countries,
suggest that cardiovascular disease will become a leading cause of death in
patients with HIV even in limited-resource settings, stressing how much crucial
is a thorough knowledge and understanding of cardiac manifestations of HIV/AIDS
for any European cardiovascular specialist.
In such a complex yet not completely understood scenario, interaction among
traditional risk factors, comorbidities, antiretroviral medications and the
pro-inflammatory role of HIV emerges and it represents a novel interplay in
the key model of infectious agent-host environment.
Short term benefits of specific antiretrovirals prevent cardiovascular disease
in HIV patients, but long term benefits need more data and longer-term follow-up
to be correctly assessed. The results of ongoing trials will provide important
information on how to manage timing of HAART initiation with the ultimate goal
of optimizing the risk-benefit balance. The START trial includes antiretroviral-naive
HIV-positive people with CD4 counts greater than 500 cells/mm3. It is taking
place in about 90 sites in nearly 30 countries where participants are randomized
to either receive antiretroviral treatment immediately or to defer treatment
until their first CD4 count less than 350 cells/mm3 or they have clinical signs
of advanced HIV disease. Such a randomized study will therefore address the
question if the purported benefits of early therapy (as it is suggested by U.S.
Department of Health and Human Services - DHHS guidelines) may overcome the
expected drug-associated side-effects.
Others challenges and open issues remain concerning the best time to start antiretroviral
therapy, the best regimen in patients with established coronary artery disease
(CAD), the role of anti-inflammatory and anti-thrombotic drugs as well as the
long-term clinical outcomes in HIV-positive patients, previously considered
“doomed”, and now predicted to live longer and face age-related morbidities.
writed at 17-10-2013 00:15:47